A tendency toward schizophrenia may originate during the first month of fetal development, according to researchers who grew “mini-brains,” or organoids, to find a possible genetic basis for the disorder.
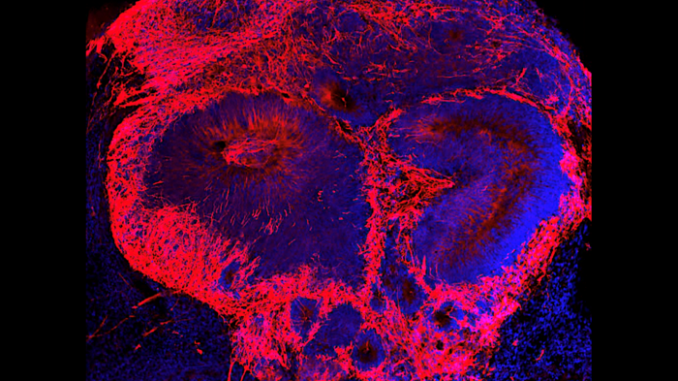
Investigators at Weill Cornell Medical Center conducted a study, published in Molecular Psychiatry, on the many changes human brain cells undergo during the first month of embryonic development. The researchers used stem cells from schizophrenia patients and control participants to grow organoids in a laboratory and compared the two groups.
They found that a reduced expression of two specific genes in the cells hinders early development and causes a shortage of brain cells in organoids grown from schizophrenia patients’ stem cells. The researchers obtained stem cells from adult donors to avoid ethical concerns over the use of embryonic stem cells.
“This discovery fills an important gap in scientists’ understanding of schizophrenia,” said co-author Dilek Colak, a neuroscientist at Weill Cornell Medicine. While schizophrenia typically only becomes evident in adults, studies of the brains of deceased people with the disease show cavities called ventricles, as well as differences in the upper layers of the brain that probably occurred earlier.
“There were hints [that] schizophrenia started during early development, but we didn’t have proof,” Colak said.
The research team collected stem cells from 21 donors and grew brain tissue matching each patient’s genetic make-up. They then used single-cell RNA sequencing to compare gene expression in individual cells in the patients’ tissue and in tissue grown from people without schizophrenia. “We found a common pathology among all the patients with schizophrenia despite each of the patients having distinct disease presentations,” Colak said.
The study found that samples from schizophrenia patients showed reduced expression of BRN2, a regulator of gene expression, and pleiotrophin, a cell-growth promoter. This caused reduced production of new brain cells and increased brain-cell death. Researchers determined that replacing the missing BRN2 in the cells restored brain cell production and adding pleiotrophin reduced brain-cell death.
“We’ve made a fundamental discovery providing what we think is the first evidence in human tissue that multiple cell-specific mechanisms exist and likely contribute to [the] risk of schizophrenia,” said lead author Michael Notaras. “This forces us, as a field, to reconsider when disease truly begins and how we should think about developing the next generation of schizophrenia therapeutics.”
The researchers believe that further study could confirm their results and lead to therapies to correct genetic differences in specific brain cell types.
Colak and the other researchers used the mini-brains to understand the roles of each cell type and the genetic factors interacting with the environment to cause schizophrenia. Currently, their focus is on endothelial cells, which line blood vessels and release important cytokine molecules, promoting an immune response. Mini-brains developed from schizophrenia patients showed an excess of early endothelial-related cells, which could lead to an excessive immune response.
“This may explain the link between maternal infections during pregnancy and schizophrenia seen in mouse studies,” Colak said.
Edited by Siân Speakman and Kristen Butler
Recommended from our partners
The post Origins Of Schizophrenia May Be Found In Early Embryonic Development appeared first on Zenger News.

